Behind the Study: ONC201, TRAIL, and Breast Cancer
Oncotarget, Spotlight
July 5, 2021Behind the Study is a series of transcribed videos from researchers elaborating on their recent oncology-focused studies published by Oncotarget. A new Behind the Study is released each Monday. Visit the Oncotarget YouTube channel for more insights from outstanding authors.
—
Founding Oncotarget Editorial Board Member, Dr. Wafik S. El-Deiry, and recent MD/PhD graduate of Temple University, Dr. Marie D. Ralff, discuss their 2020 study published by Oncotarget entitled, “TRAIL receptor agonists convert the response of breast cancer cells to ONC201 from anti-proliferative to apoptotic.”
Dr. Wafik El-Deiry
We’re grateful for the opportunity to talk a little bit about our paper. I am Wafik El-Deiry. I’m a physician scientist, a medical oncologist, professor at Brown University, director of the Cancer Center at Brown University, and Associate Dean at the Warren Alpert Medical School. I’m here with my colleague Marie Ralff who will introduce herself as well.
Dr. Marie Ralff
Hi, my name is Marie Ralff. I’m an MD-PhD student. I just graduated from Temple a couple of weeks ago and I was in Dr. El-Deiry’s lab from 2015 to 2019, and this paper is a result of some of the work that I did there.
Dr. Wafik El-Deiry
Thank you Marie. The paper we’re going to discuss today is entitled, “TRAIL receptor agonists convert the response of breast cancer cells to ONC201 from anti-proliferative to apoptotic” and the first author is Dr. Ralff. And Marie said, we started this work at Fox Chase Cancer Center and we finalized some experiments after we moved to Brown University right at the beginning of 2019. But before we get into the details of the actual experiments we did in this manuscript, let me just take you back a little bit to provide some background that sets the stage for the work that we pursued.
And so, as I said earlier, I am a medical oncologist. So for years, I’ve been interested in understanding the process of cell death as it relates to cancer and the effects of cancer treatments that we use, whether that is chemotherapy or radiation or other targeted therapies. And so in the process of trying to learn about that, going back now to the mid to late ’90s, my laboratory discovered a gene that encodes a protein called death receptor 5.
And death receptor 5 is a protein that sits in the cell membrane and is engaged by a ligand protein that circulates that is made by natural killer cells, for example. And it’s part of our innate immune system for how our body suppresses cancer and its metastases. And so for almost 25 years now, we have been interested in this cell death immune mechanism that suppresses cancer in our body and how various therapeutics interact with this pathway to have anti-cancer effects in patients or in the laboratory, in the different models that we study.
And because this is a powerful way that cancer can be suppressed, along the way we had the idea of looking for small molecule drugs that can activate this immune mechanism of cancer suppression. And so back in 2007, while we were at University of Pennsylvania, we carried out a chemical library screen in my laboratory, looking for small molecules that upregulate the TRAIL gene with the idea that the increased production of TRAIL by small molecules, whether they’re normal cells or tumor cells, could have a therapeutic benefit in the treatment of cancer.
And we found a number of small molecules at the time, one of which has come to be known as TIC10, for TRAIL-inducing compound, number 10. And this compound entered clinical trials under the name of ONC201. And interestingly, the compound has been having effects on tumors in patients, including patients with aggressive brain tumors, midline brain tumors with a specific epigenetic defect, H3K27M, and has been under study in other clinical trials. There have been some effects of the compound seen in patients with prostate cancer where bone metastases have shrunk or visceral metastases have lost their PET avidity. And some patients with metastatic endometrial cancer have had responses in their lymph nodes or in lung metastases.
And so the drug continues to be studied in the clinic. So we have been interested to understand more about exactly how this drug is working in patients, as well as in our preclinical models, trying to think of ways of getting the drug to work better in combination with other therapeutics, and trying to gain insights into when we use this drug, why doesn’t it work across the board for all tumors in the same way? We appreciate there is a heterogeneity in cancer that we are learning about, the whole field is learning about this, but the question is with this specific drug: What is the pattern of response? What determines that? How can we get it to work a little bit better?
So by way of just a little bit more background, while we originally described the discovery of this compound in a Science Translational Medicine paper we published in 2013. In that paper, we describe TIC10, TRAIL-inducing compound number 10, is able to activate the TRAIL gene by effects on some kinases within the cell, such as AKT and ERK, which individually phosphorylate a transcription factor called FOXO3a. And when this transcription factor is phosphorylated, it is retained in the cytoplasm. And when these kinases are inhibited, the transcription factor then translocates to the nucleus, binds to the TRAIL gene, and activates TRAIL.
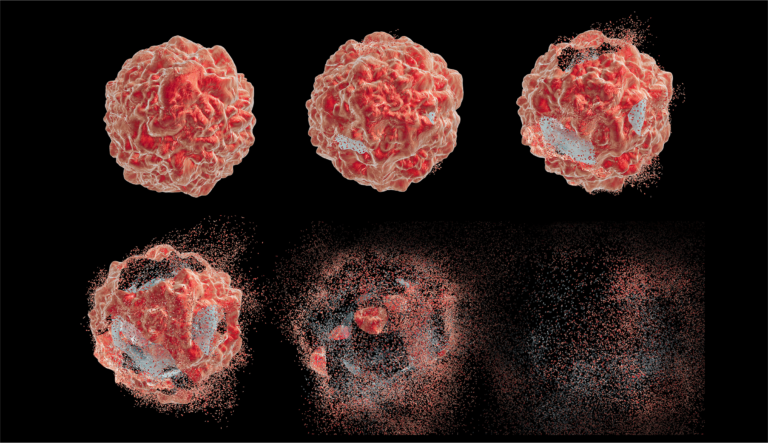
So, we showed these effects early on including some in vivo effects. And one of the interesting things that we observed early on was that the timing of cell death culture or in vivo was somewhat delayed. It took two-to-four days to see significant cell death. And we knew from our earlier studies with TRAIL, if you add TRAIL to tumor cells, if they’re sensitive, they just melt away and are obliterated within just a few hours. Like three-to-four hours in many systems, those cells are dead and gone.
So we were interested in why it was taking so long. What are some of the earlier events? And so we published a second paper in 2016 in Science Signaling where we gained insights into some of those early events. And the insight that we gained was that ONC201/TIC10 activates what’s referred to as an integrated stress response in tumor cells, and that this involves kinases. We looked at a bunch of kinases that mediate this signaling, and we uncovered HRI and PKR as relevant kinases that are involved in activation of eIF-2 alpha, ATF4, CHOP, transcription factors, and then ultimately production of death receptor 5 as a transcriptional target.
So this was interesting for several reasons. One of the main reasons is that the original discovery of TIC10/ONC201 was based on its ability to upregulate TRAIL, this art of the host immune system that suppresses cancer and its metastases. And here we just also discover that this small molecule can upregulate the integrated stress response leading to production of death receptor 5, the receptor for TRAIL.
And so we think that the regulation of TRAIL and death receptor 5 is relevant and significant part of the mechanism of action of this new anticancer compound recognizing. I’ll ask Marie to set the stage for her paper and then get into our findings, but one of the observations we made in that 2016 Science Signaling paper is that the effects of ONC201/TIC10 on a large number of human tumor cell lines shows heterogeneity. So, do you see pro-apoptotic effects in a number of human tumor cell lines?
But in other cases, we saw anti-proliferative effects and that was interesting. When you discover a candidate therapeutic, you want to learn more about it in terms of its effects just so that everyone understands what it does and how it does it, but also issues with how could we modulate these responses or examples from anti-proliferative to pro-apoptotic, which would be a desirable thing in a clinical context where one would hope to see tumor shrink and antitumor effect without much toxicity. So, in drug development, we want to make sure we’re having an effect on the tumor without much toxicity.
One of the interesting aspects of ONC201 is that the drug is extremely well-tolerated. When it entered clinical trials, it’s a pill started in the clinic on an every three week schedule and was having effects on brain tumors under that schedule.
Later on, we published the second paper in the Journal of Clinical Investigation in 2018 where we intensified the dose of ONC201, and were able to show an effect on metastasis as well as prolonged pathway suppression in vivo along the lines of the AKT and ERK suppression that I described earlier. And those results led to a modification of how the drug is being tested in clinical trials on a weekly schedule. And the drug was being developed by a company called Oncoceutics, that I founded over 12 years ago, that has been taking this compound into the clinic and testing its effects in various tumor types.
A little bit of background about TRAIL in breast cancer, because this is the focus of our paper here. And just to set the stage for Marie, TRAIL was discovered around 1994-95, and that discovery provided a new way to potentially treat cancer. TRAIL is part of the tumor necrosis family of cytokines. And years ago, when I was in clinical training at Johns Hopkins, there were clinical trials testing TNF (or tumor necrosis factor) in combination with other drugs for patients with cancer.
The problem was not that TNF is not effective, TNF is really an effective therapeutic, however, it’s also incredibly toxic because of its effects on NF-kappa B and has really been abandoned for systemic administration. But when TRAIL came along, it doesn’t have much of an effect on NF-kappa B and it preferentially kills tumor cells or transforms cells or by the way, virally infected cells, but not normal cells. So that was part of its excitement, lack of toxicity, lack of this systemic inflammatory response.
And TRAIL was tested in the clinic for a number of years. And there were some responses in some tumors. But overall, the signal from TRAIL as an effective therapeutic was fairly weak. In part, we think because TRAIL has a short half-life. And so, we were excited with the discovery of TIC10, that we could increase TRAIL production in our mouse models or in vivo or in humans to potentially upregulate this TRAIL pathway and boost the immune system to have antitumor effects.
As anyone who has treated cancer knows, cancer is complex. And again, going back to this major heterogeneity of what we see when we treat tumor cells with drugs, we see this heterogeneity with ONC201. So we’ve wanted to understand that in terms of what happens in different cells and what could we do about it to get a more favorable therapeutic outcome.
So with that very long winded introduction, I hope you have an understanding where we have been with the work on the TRAIL pathway and ONC201/TIC10 discovery and development. I’ll turn it over to Marie to talk about her work in the lab including a prior paper that let us to the current paper. So, Marie…
Dr. Marie Ralff
Thanks Dr. El-Deiry. That was really helpful. So now hopefully everyone can get an idea of some of the history of TRAIL and the history of ONC201 in the lab. I joined the lab as a PhD student in 2015, and I picked up a project that focused specifically on the effects of ONC201 in breast cancer. And Dr. El-Deiry was alluding to my first paper published in 2017 in Molecular Cancer Therapeutics. This was the first paper to demonstrate the efficacy of ONC201 in breast cancers from a wide range of molecular subtypes.
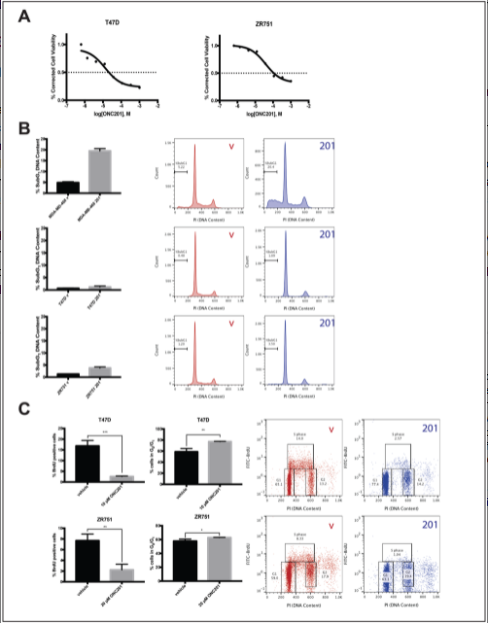
Breast cancers, in general, are pretty TRAIL-resistant tumor type. There is only a small subset of the triple negative breast cancers which actually show sensitivity to TRAIL. Majority are very resistant. So it was promising to see that when we treated breast cancers from a variety of different molecular subtypes with ONC201, the compound had efficacy. And looking a little bit more closely into that, some of these tumor types, the triple negative one specifically, the compound was having a pro-apoptotic effect. In other tumor types, it was having an anti-proliferative effect.
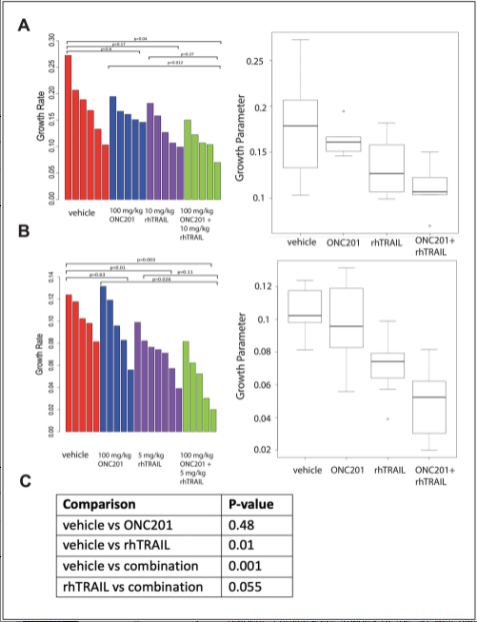
The anti-proliferative effect involved an arrest in the g1 phase of the cell cycle. And when we looked in vivo, we saw that while the pro-apoptotic effect translated into efficacy in a mouse model of breast cancer, the anti-proliferative effect did not. So this got us thinking that we should search for a strategy that could be used to convert this anti-proliferative effect into an apoptotic one.
Now, Dr. El-Deiry talked a little bit about the effects of ONC201 on DR5, the cell surface TRAIL receptor – one of the death receptors – and I don’t believe that he mentioned (this), but there are also effects of the compound on anti-apoptotic proteins. And so our knowledge of these two things, two known mechanisms of TRAIL resistance in breast cancer, led us to hypothesize that the combination of ONC201 and a TRAIL receptor agonist may be highly efficacious. So we found that this indeed was the case. That if we pretreat TRAIL resistant breast cancer cells with ONC201, the level of surface death receptor 5 goes up and the intracellular levels of anti-apoptotic proteins go down, thereby priming the cells to undergo death through the TRAIL pathway. So if we then add in a TRAIL receptor agonist, it induces apoptosis in a very potent way.
Dr. Wafik El-Deiry
I think the highlights that I would like you to go through, Marie, would be the issue of trying to convert anti-proliferative to pro-apoptotic, the concept of priming the cells. So think about it this way: DR5 goes up, the anti-apoptotic proteins go down, but the cells are not really sensitive to the drug and they’re not really sensitive to the TRAIL. So we wondered, at some point, why the cells are not responding to the drug. We suspected, well, maybe they don’t make enough TRAIL. Describe this as a TRAIL-inducing compound. So we started to think, okay, well, what if we add some TRAIL or a death receptor agonist antibody? And so we did that.
Then we interrogated that mechanism. And I think it’s important to point out that there’s a dependence on death receptor 5. There are a couple of points that I think are really nice to make, and I would love to do that. One is this idea of a switch, and we’ve talked about this in the past, the idea of flipping a switch. The concept is cells are treated with the small molecule compound, not a whole lot has happened. Cells are treated with TRAIL, not a whole lot has happened. You put them together and it’s like flipping a switch. The cells now undergo potent cell death.
Your cell culture data shows this beautifully in at least four different human breast cancer cell lines. I think that’s important to say. I think the idea that it’s not toxic to the fiber blasts is worth mentioning. I think the idea that the natural killer cells are active against the breast cancer cells that have been exposed to ONC201 is nice, and then the in vivo study. So I would just review all of that. Take your time because all of these are nice points to make. To illustrate the progression of thinking, the idea combination therapy, the potential efficacy, and open clinical trials, for example, at the National Cancer Institute, to look at ONC201 in breast cancer.
And our work would basically predict that it would be a rare patient with breast cancer who might just outright respond to this drug. And again, this goes back to cancer is complex and drug development is also very hard. And our colleagues, including at places like the National Cancer Institute, may be discouraged by single agent activity or the lack thereof in breast cancer. And here we are with this very nice preclinical data that rides hope or actually moving this forward, and we’ll get to the future directions, but I think we build on what we know. There are hurdles, challenges, and I see this work as an overcoming of some of those challenges through basic science and rational thinking, and rational combination of therapeutics based on molecular pathways. So I would say all of that.
Dr. Marie Ralff
We also showed that this combination of ONC201 with TRAIL receptor agonists was non-toxic to human fibroblast. And our in vivo studies, as well, confirmed that the combination was very safe in mice.
Dr. Wafik El-Deiry
Talk about the dependence on DR5 and also the efficacy on tumor growth in vivo besides the safety.
Dr. Marie Ralff
We showed that the upregulation of DR5 by ONC201 was necessary for this sensitization to TRAIL receptor agonists. The benefit here was that ONC201 alone had the potential to have efficacy in the triple negatives, but ONC201 alone was never going to work in non triple negatives, whether it be HER2 amplified or ER/PR-positive.
Dr. Wafik El-Deiry
Well, that’s only partially correct because in some of the triple negatives it doesn’t do anything. And I strongly suspect that in those other triple negatives, the combo will bring out an effect. So…
Dr. Marie Ralff
I know your thinking there is that there’s less treatment options for triple negative in general, so it’s like a way to, you know…
Dr. Wafik El-Deiry
Anyways, the fact is your paper is… that figure in your paper is with non ER/PR-positive, they have to have HER2. I would say it. And we had talked about obviously doing more of this in triple negative than we had time to do, but it does go beyond just hormone receptor positive. And, as you know, hormone receptor positive breast cancer generally has much better outcomes and lots of treatment options. Like you said, the triple negative is where we really need to make important progress, but I think progress in breast cancer in general will ultimately be very helpful.
Thank you Marie, for that great summary of the data in the paper. And so just to summarize, we find that the combination of ONC201 with TRAIL or TRAIL receptor agonist antibodies is a potent synergistic combination that appears to have preclinical efficacy in breast cancer and does have some immune stimulatory effects that we showed in this paper.
This is a novel therapeutic strategy that we plan to pursue and try to bring into the clinic because it could make a difference. Based on our preclinical results, it isn’t clear how ONC201 monotherapy will play out in clinical trials. And that consideration of combination therapies, such as with this one, might increase the chances for therapeutic efficacy in the clinic in different breast cancer subtypes. This type of insight is coming from detailed molecular analysis of breast cancer cell lines and in vivo models, and with an understanding of the mechanism of action of ONC201/TIC10 that involves upregulation of TRAIL and death receptor 5. Although in a number of human cell lines there isn’t enough TRAIL production, and so the addition of extra TRAIL helps trigger the apoptotic cell death. It’s almost like a switch that when you combine these two agents, you trigger cell death where individual agents just are not triggering that pro-apoptotic cytotoxic response.
I should say that at this point, I want to make a couple of comments. One, to acknowledge the funding of our work through the NIH and the National Cancer Institute and through the American Cancer Society. Support of our work, I would like to acknowledge our co-authors: Aakash Jhaveri, Jocelyn Ray, Lanlan Zhou, Avital Lev, Kerry Campbell, Dave Dicker, and Eric Ross. Some of our colleagues are from Fox Chase Cancer Center where the work was started and largely completed by Marie, who was the first author.
And because we have seen these effects of the combination of TRAIL plus ONC201 as a promising therapeutic combination, one of the extensions of the work that follows naturally is the question of: How does this work in other tumor types?
What has been observed in the clinic with ONC201 monotherapy are these remarkable responses in brain tumors, but not so much in other solid tumor types. So could a combination like ONC201 and TRAIL or TRAIL receptor agonists be worth pursuing in the clinic to achieve synergistic antitumor efficacy? And so we have a number of other results and other systems, some by our co-authors here. Aakash Jhaveri as part of his master’s thesis work at Brown University, looked at combinations of ONC201 with TRAIL or another investigational drug called TLY012 as well as some combinations of the ONC201 analog, ONC212, with TLY012 in pancreatic cancer models.
Jocelyn Ray, who is in the GYN oncology residency program at Temple Fox Chase, looked at the efficacy in preclinical models of the ONC201 TRAIL combination in endometrial cancer models. So we have a couple of manuscripts that are on the way.
We presented this work at national meetings such as AACR and some other society meetings, and we do see efficacy in other systems. We do have some ongoing work at Brown University being conducted by Dr. Cassandra Parker, who is a resident in the department of surgery looking at gastric cancer models, where we are seeing similar synergy between ONC201 and TRAIL, and similar in vivo synergy in gastric cancer with the combination of ONC201 and TLY.
So we think that the insights gained in the work done by Dr. Ralff as presented in this paper, sets the stage for future translational clinical trials in the area of breast cancer, as well as other tumors, where we could trigger activation of the death receptor pathway that is part of the innate immune system for suppression of cancer and its metastases.
So we thank you for your attention to our presentation this afternoon and we look forward to seeing our own progress as well as collaboration with colleagues around the country, and around the world as we bring these therapeutics into clinical translation. Thank you.
Click here to read the full study published by Oncotarget.
YOU MAY ALSO LIKE: More Oncotarget Videos on LabTube
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.